As we enter the 4th year of the COVID-19 pandemic and as the number of infected survivors grows ever larger, attention is increasingly turning to the risks of long COVID and reinfection.
Characteristics of Long COVID
Most patients totally recover from acute COVID within 3 to 4 weeks after onset of infection. Long COVID has been reported in 10% to 30% of those with COVID-19,1 and in some studies, even more. It is more common in women, non-whites, hospitalized patients and those with a COPD and/or smoking history. The World Heath Organization characterizes Long COVID, or Post COVID-19 Syndrome, as being associated with:
• Individuals with a history of probable or confirmed SARS-CoV-2 infection (the virus that causes COVID-19) who experience symptoms impacting everyday life, such as fatigue, shortness of breath and cognitive dysfunction; and
• Symptoms that usually are present 3 months from the onset of acute COVID-19, that last for at least 2 months and can’t be explained by an alternative diagnosis.
Interestingly, most with post-COVID syndrome are PCR negative, i.e., they have biologically recovered from acute COVID.2 Approximately 25% of Americans with long COVID report significant activity limitations.3
Reinfection Risk
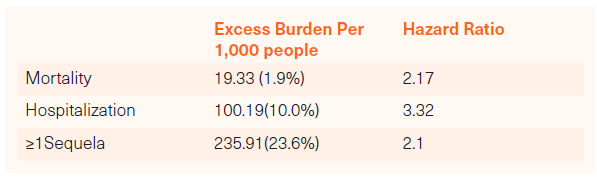
Those infected more than once with SARS-CoV-2 have a higher risk of experiencing diseases associated with long COVID. However, the severity of disease in reinfected people appears to be relatively mild in comparison to those infected only once. A recent V.A. study compared 40,947 people with 2 or more SARS-CoV-2 infections with 443,588 people with only one infection, measuring excess burden and hazard ratios 6 months after reinfection.4
Excess Burden and Hazard Ratios in reinfected versus singly infected people was as follows:
Excess Burden and Hazard Ratios for specific impairment groupings measured were as follows:
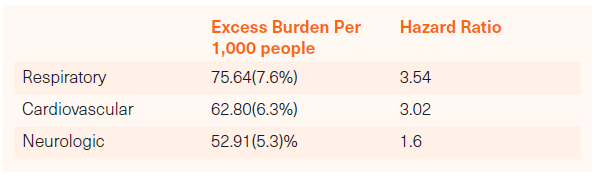
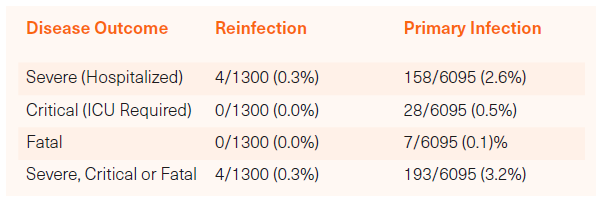
Although people with multiple SARS-CoV-2 infections clearly have a higher incidence of respiratory, cardiovascular and neurologic impairments, the severity of the reinfection related impairments is less than that associated with primary infection. A study published in the New England Journal of Medicine (NEJM) found that people experiencing a single infection only experienced severe, critical or fatal disease at more than 10 times the rate of those experiencing multiple infections.5
The NEJM study was based on a younger, healthier cohort of subjects and therefore not entirely representative of the larger COVID positive population. Nevertheless, the comparative data is directionally instructive:
Severity of Reinfection versus Primary Infection
Number with Disease Outcome/Total in Study:
Conclusions
We continue to learn more about the long-term risks of COVID-19, but more is still unknown than known. We know that the risk for hospitalized patients is greater, more so for ICU patients. Comorbidities matter and increase risk, particularly COPD and other respiratory impairments. Reinfection increases the risk of impairments, but with diminished potency. We will continue to follow and report on the evolving research.
Mike Fasano is CEO at Fasano Associates
Footnotes:
1Nashville Chest, 2022, Oct 16-19
2Clinical Research & Reviews, 15(3), 869-875
3CDC Survey, Sep. 14-26, 2022
5New England Journal of Medicine 2021; 385:2487-24-89
Any views expressed in this article are those of the author(s) and do not necessarily reflect the views of Life Risk News or its publisher, the European Life Settlement Association